The most common causes of low back pain are spinal diseases, mainly degenerative dystrophies (osteochondrosis, deforming spondylosis) and excessive tension in the back muscles.In addition, various diseases of the abdominal and pelvic organs, including tumors, can cause the same symptoms as a herniated disc compressing the spine.
It is no coincidence that these patients turn not only to neurologists, but also to gynecologists, orthopedists, urologists and, of course, most importantly to local or family doctors.
Causes and pathogenesis of low back pain
According to modern beliefs, the most common causes of low back pain are:
- Pathological changes in the spine, mainly degenerative dystrophy;
- Muscle pathological changes, the most common being myofascial syndrome;
- Pathological changes in abdominal organs;
- Neurological disorders.
Risk factors for low back pain are:
- strenuous physical activity;
- Uncomfortable working posture;
- Injuried;
- cooling, airflow;
- alcoholism;
- depression and stress;
- Occupational diseases related to exposure to high temperatures (especially in hot workshops), radiant energy, sudden temperature fluctuations, and vibration.
Vertebral causes of low back pain include:
- Root ischemia (discogenic radiculopathy, discogenic radiculopathy), caused by disc herniation compressing the root;
- Reflex muscle syndrome, which may be caused by degenerative changes in the spine.
Various dysfunctions of the lumbar spine have a certain impact on the occurrence of low back pain. Due to incorrect posture, intervertebral joints are blocked and mobility is impaired.In the joints located above and below the block, compensatory overactivity occurs, causing muscle spasms.
Signs of acute spinal canal compression
- numbness in the perineum, weakness and numbness in the legs;
- Retention of urination and defecation;
- As the spinal cord becomes compressed, the pain decreases, followed by numbness in the pelvic girdle and extremities.
Low back pain in childhood and adolescence is most often caused by abnormal spinal development.Spina bifida (spina bifida) affects 20% of adults.Examination revealed hyperpigmentation, birthmarks, multiple scars, and hyperkeratosis in the lumbar skin.Urinary incontinence, nutritional disorders, and leg weakness sometimes occur.
Low back pain can be caused by lumbarization (the transition of the S1 vertebrae relative to the lumbar spine) and sacralization (the attachment of the L5 vertebrae to the sacrum).These abnormalities develop due to individual characteristics of the development of the transverse processes of the vertebrae.
disease classification form
Almost all patients complain of lower back pain.The disease mainly manifests as inflammation of low-lying movable joints (intervertebral joints, costovertebral joints, lumbosacral joints) and spinal ligaments.Gradually, the spine ossifies, loses elasticity and mobility, becomes as fragile as a bamboo pole, and is easily injured.In the obvious clinical stage of the disease, the mobility of the chest and the vital capacity of the lungs during breathing decrease significantly, leading to the occurrence of many lung diseases.
spinal tumors
A distinction is made between benign and malignant tumors, primarily originating in the spine and metastatic tumors.Benign tumors of the spine (osteochondromas, enchondromas, hemangiomas) are sometimes clinically asymptomatic.With hemangiomas, spinal fractures can occur even with minor external influences (pathological fractures).
Malignant tumors are mostly metastatic tumors that originate from organs such as the prostate, uterus, breast, lung, and adrenal glands.Pain in this condition is more common than in benign tumors—it is often constant, painful, aggravated by the slightest movement, and prevents the patient from resting and sleeping.It is characterized by a gradual worsening of the condition, increased general fatigue, and noticeable changes in the blood.X-rays, computed tomography, and magnetic resonance imaging are important for diagnosis.
osteoporosis
The main cause of the disease is a decrease in the function of the endocrine glands due to independent diseases or in the context of general aging of the body.Osteoporosis may occur in patients taking long-term corticosteroids, amazine, antituberculosis drugs, and tetracyclines.Nerve root disease that accompanies back pain is caused by deformation of the intervertebral foramina, and spinal disease (myelopathy) is caused by compression of the radiculomedullary arteries or vertebral fractures, even after minor injuries.
myofascial syndrome
Myofascial syndrome is a leading cause of back pain.It can occur due to overexertion (during strenuous physical activity), overstretching and bruising of muscles, unphysiological postures at work, reaction to emotional stress, shortening of one leg or even flat feet.
Myofascial syndromes are characterized by the presence of so-called "trigger" zones (trigger points), and pressure on the trigger zone causes pain that often radiates to adjacent areas.In addition to myofascial pain syndrome, the cause of pain may also be the inflammatory muscle disease called myositis.
Low back pain is often caused by internal organ diseases: gastric and duodenal ulcers, pancreatitis, cholecystitis, urolithiasis, etc.The symptoms can be obvious and resemble those of low back pain or discogenic lumbosacral radiculitis.However, there are clear differences that distinguish referred pain from pain due to peripheral nervous system disease, which is due to symptoms of the underlying disease.
Clinical symptoms of low back pain
Most commonly, low back pain occurs between the ages of 25 and 44 years.There is acute pain, which usually lasts 2-3 weeks and sometimes up to 2 months, and there is chronic pain - more than 2 months.
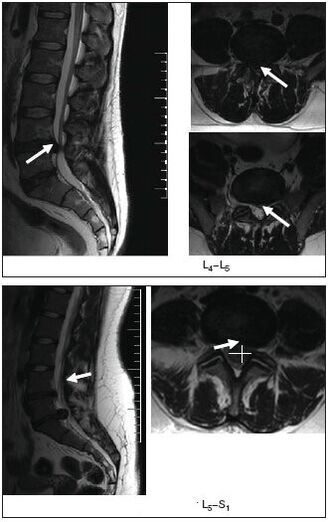
Compressive radiculopathy (discogenic radiculopathy) is characterized by a sudden onset, usually after heavy lifting, sudden movement, or hypothermia.Symptoms depend on the location of the lesion.The syndrome occurs based on compression of the tooth roots by disc herniation, which is the result of degenerative processes due to static and dynamic loads, hormonal imbalances and injuries, including microtrauma to the spine.Most commonly, the pathological process involves the spinal root region from the dura mater to the intervertebral foramen.In addition to disc herniation, bone growth, scarring changes in the epidural tissue, and hypertrophic ligamentum flavum may also be associated with root trauma.
The upper lumbar roots (L1, L2, L3) are rarely affected: they account for no more than 3% of all lumbar radiculopathy syndromes.The L4 root is involved twice as frequently (6%), resulting in characteristic clinical manifestations: mild pain on the lower and anterior surfaces of the thigh and medial surface of the calf, abnormal sensation in the area (numbness, burning, crawling sensation); mild quadriceps weakness.Knee reflexes are preserved and sometimes even enhanced.The L5 root was most commonly affected (46%).The pain is localized to the lumbar and buttock area, along the outer surface of the thigh, the anterior outer surface of the calf, to the foot and III-V fingers.It is usually accompanied by decreased sensitivity of the skin on the anterior outer surface of the leg and decreased strength of the extensor muscles of the third to fifth fingers.The patient finds it difficult to stand on his heels.Long-standing radiculopathy can lead to atrophy of the tibialis anterior muscle.S1 roots were also frequently affected (45%).In this condition, pain in the lower back radiates along the outer rear surface of the thigh, the outer surface of the calf, and the foot.Examination often reveals hypoalgesia on the posterior outer surface of the leg and decreased strength of the triceps and toe flexors.Such patients have difficulty standing up.Achilles tendon reflexes are weakened or lost.
Vertebral lumbar reflex syndrome
It can be acute or chronic.Acute low back pain (LBP) (low back pain, "low back pain") occurs over a period of minutes or hours, often suddenly due to improper movement.Stinging, shooting pain (like an electric shock) concentrated throughout the lower back, sometimes radiating to the iliac area and buttocks, acutely aggravated by coughing or sneezing, and relieved by lying down, especially when the patient finds a comfortable position.Limited movement of the lumbar spine and tightness of the lumbar muscles cause Lasegue symptoms, which are often bilateral.Therefore, the patient lies on his back with his legs extended.The doctor simultaneously bends the knee and hip joints of the affected leg.This does not cause pain because the diseased nerves relax when the leg is in this position.The doctor then bends the leg at the hip-femoral joint and begins to straighten it at the knee, causing tension on the sciatic nerve, causing severe pain.Acute low back pain usually lasts 5-6 days, sometimes less.The first attack ends faster than subsequent attacks.Recurrent episodes of low back pain often develop into chronic low back pain.
atypical low back pain
Back pain caused by degenerative changes in the spine or myofascial syndrome has many atypical clinical symptoms.These signs include:
- Pain occurs in childhood and adolescence;
- Injury to the back shortly before the onset of low back pain;
- Back pain accompanied by fever or signs of intoxication;
- spine;
- Pain in the rectum, vagina, legs, and waistband;
- Low back pain is related to eating, defecation, sexual intercourse, and urination;
- nonecological pathology (amenorrhea, dysmenorrhea, vaginal discharge), which appeared against the background of lower back pain;
- Pain in the lower back worsens in the horizontal position and decreases in the vertical position (Razdolski syndrome, characteristic of neoplastic processes in the spine);
- Pain that gradually worsens over one to two weeks;
- Appearance of limbs and pathological reflexes.
Examination method
- External examination and palpation of the lumbar region to identify scoliosis, muscle tension, pain, and trigger points;
- Determine the range of motion of the lumbar spine and areas of muscle atrophy;
- Neurological status examination; determination of catatonic symptoms (Lassegue, Wasserman, Neri).[Study of Wasserman's symptoms: Bending the leg at the knee joint causes thigh pain in patients in the prone position.Neri Symptom Study: A patient lying on their back with legs straight, with the head sharply bent toward the chest, causes severe pain in the lower back and along the sciatic nerve.
- Study of sensitivity status, reflex bulbs, muscle tone, vegetative disorders (swelling, changes in skin color, temperature and humidity);
- Radiographic, computerized, or magnetic resonance imaging of the spine.
MRI is particularly informative
- Ultrasound examination of pelvic organs;
- Gynecological examination;
- If necessary, additional tests are performed: cerebrospinal fluid, blood and urine, sigmoidoscopy, colonoscopy, gastroscopy, etc.
treat
Acute low back pain or worsening of vertebral or myofascial syndrome
Indiscriminate treatment.Gentle motor mode.If severe pain occurs on the first day, rest in bed and then walk with a cane to reduce the load on your spine.The bed should be hard and a wooden board should be placed under the mattress.To keep warm, wool shawls, electric heating pads and heated sand or salt bags are recommended.Ointments with beneficial effects include: finalgon, tiger, capsin, diclofenac, etc., as well as mustard ointment, pepper ointment, etc.Erythematous doses of ultraviolet radiation, leeches (taking into account possible contraindications), and irrigation of the painful area with ethyl chloride are recommended.
Electrotherapy has analgesic effects: transcutaneous electrical analgesia, sinusoidal modulated current, dynamic current, novocaine electrophoresis, etc.Use of reflexology (acupuncture, laser therapy, cautery) is effective; novocaine blocks, trigger point pressure massage.
Medication includes analgesics, nonsteroidal anti-inflammatory drugs; sedatives and/or antidepressants; and drugs that reduce muscle tension (muscle relaxants).If arterial hypotension occurs, tizanidine should be used with caution due to its hypotensive effect.If swelling of the spine is suspected, administer a diuretic.
The main analgesic medications are nonsteroidal anti-inflammatory drugs, which are often used uncontrollably by patients when pain worsens or recurs.It should be noted that long-term use of NSAIDs and analgesics increases the risk of complications from such treatments.Currently, a variety of NSAIDs are available.For patients with spinal pain, the preferred "non-selective" agent is diclofenac 100-150 mg/day due to availability, effectiveness, and lower likelihood of side effects (gastrointestinal bleeding, dyspepsia).Oral, IM, rectal, topical, ibuprofen and ketoprofen 200 mg PO and topical, and "elective" medications - meloxicam PO 7.5-15 mg/day, nimesulide PO 200 mg/day.
Side effects may occur during treatment with NSAIDs: nausea, vomiting, loss of appetite, upper abdominal pain.May produce ulcerative effects.In some cases, gastrointestinal ulceration and bleeding may occur.Additionally, headache, dizziness, drowsiness, and allergic reactions (rash, etc.) have been noted.Treatment is contraindicated in gastrointestinal ulcers, pregnancy and lactation.To prevent and reduce indigestion symptoms, it is recommended to take NSAIDs and drink milk before or after meals.Furthermore, as has been observed in the long-term treatment of many chronic diseases, taking NSAIDs when pain worsens, along with other medications the patient is taking to treat concomitant illnesses, can lead to decreased treatment compliance and, thus, insufficient therapeutic efficacy.
Therefore, modern conservative treatment methods include the mandatory use of drugs with chondroprotective, cartilage-stimulating effects and better therapeutic effects than NSAIDs.The drug Teraflex-Advance fully meets these requirements and is an alternative to NSAIDs for the treatment of mild to moderate pain.One capsule of Teraflex-Advance medication contains 250 mg of glucosamine sulfate, 200 mg of chondroitin sulfate, and 100 mg of ibuprofen.Chondroitin sulfate and glucosamine are involved in the biosynthesis of connective tissue, helping to prevent cartilage destruction processes and stimulate tissue regeneration.Ibuprofen has analgesic, anti-inflammatory and antipyretic properties.Its mechanism of action is due to the selective blocking of cyclooxygenase (COX type 1 and type 2), the main enzyme of arachidonic acid metabolism, resulting in reduced prostaglandin synthesis.Theraflex-Advance contains NSAIDs that help increase joint range of motion and reduce morning stiffness in the joints and spine.It should be noted that, according to R.J. Tallarida et al., the presence of glucosamine and ibuprofen in Theraflex-Advance provides a synergistic effect on the analgesic effect of the latter.Furthermore, the analgesic effect of the glucosamine/ibuprofen combination was provided by a 2.4-fold lower ibuprofen dose.
After the pain is relieved, it is reasonable to switch to the drug Teraflex, which contains the active ingredients chondroitin and glucosamine.Teraflex is taken as 1 capsule 3 times daily.For the first three weeks, take 1 capsule 2 times daily.over the next three weeks.
The vast majority of patients who take Theraflex experience positive dynamics such as pain relief and a reduction in neurological symptoms.The patient tolerated the drug well and no allergic symptoms were noted.The use of Teraflex to treat degenerative spinal disease is reasonable, especially in younger patients, either in combination with NSAIDs or as monotherapy.When used concomitantly with NSAIDs, analgesia occurs 2-fold faster and the need for NSAID therapeutic doses gradually decreases.
In clinical practice, B vitamins with neurotropic effects are widely used for peripheral nervous system lesions, including those associated with spinal osteochondrosis.Traditionally, 1-2 ml of vitamins B1, B6 and B12 are administered alternately.Intramuscular injection, alternate daily.The course of treatment is 2-4 weeks.Disadvantages of this approach include the use of small doses of medication, which reduces therapeutic efficacy and the need for frequent injections.
For discogenic radiculopathy, traction therapy is used: traction (including underwater traction) is performed in a neurological hospital.For myofascial syndrome, after local treatment (novocaine block, ethyl chloride irrigation, anesthetic ointment), apply warm compresses to the muscle for several minutes.
Vertebral or myogenic chronic low back pain
If a disc herniation occurs, it is recommended to:
- Wearing a rigid corset like a "weightlifting belt";
- Avoid sudden movements and bending, and limit physical activity;
- Physical therapy to build muscle corset and restore muscle mobility;
- massage;
- Novocaine blockers;
- Reflexology;
- Physical therapy: ultrasound, laser therapy, heat therapy;
- Intramuscular vitamin therapy (B1, B6, B12), multivitamin and mineral supplements;
- For episodic pain, carbamazepine may be used.
non-pharmacological treatment
Although effective conservative treatments exist, with dozens of techniques available, some patients still require surgery.
Indications for surgical treatment are divided into relative indications and absolute indications.Absolute indications for surgical treatment are the presence of caudal syndrome, the presence of disc herniation, and severe radicular pain syndrome that does not relieve symptoms despite treatment.The development of marrow ischemia of the nerve roots also requires urgent surgical intervention, however, after the first 12-24 hours, the indications for surgery in this case become relatively small, firstly, due to the formation of irreversible changes in the roots, and secondly, because in most cases, during treatment and rehabilitation measures, the process subsides in about 6 months.The same regression period is also observed for the delayed operation.
Relevant indications include failure of conservative treatment and recurrence of sciatica.The duration of conservative treatment should not exceed 3 months.and last for at least 6 weeks.It is considered reasonable to resort to surgery within the first 3 months in cases of acute radicular syndrome and failure of conservative treatment.Prevent the root causes of chronic pathological changes after pain attacks.A relative indication is in cases of extremely severe pain syndromes, where the pain component is replaced by an increase in neurological deficit.
The proteolytic enzyme caripazine is currently widely used for electrophoresis during physical therapy.
It is well known that therapeutic physical training and massage are components of the complex treatment of patients with spinal pathologies.The goals pursued by Therapeutic Gymnastics are to comprehensively enhance body strength, increase efficiency, improve movement coordination, and enhance physical fitness.In this case, special exercises are designed to restore certain motor functions.


















